In my last blog I discussed the prospects of low-end disruptive strategy for potentially disruptive innovations in healthcare. Because low-end disruptions compete directly with established and superior incumbent offerings, the prospects, I argued, are not good. The price-insensitivity inherent in a third-party payment system diminishes the cost advantage an inferior but potentially disruptive good or service leverages against incumbents. Thus, low-end and potentially disruptive options that actually cost less than incumbent options appear no more affordable to patients, making the decision to purchase the superior incumbent an easy one. Instead, I proposed the path of new-market disruptive strategy for healthcare entrepreneurs. New-market disruptions compete with nonconsumption, as opposed to directly with superior incumbent technologies, by targeting those who for one reason or another don’t consume the existing solution. To illustrate this point, let’s consider how a potentially disruptive innovation could disrupt the traditional process of a major cardiac surgery using new market strategy.
Coronary artery bypass grafting (CABG – pronounced “cabbage”) is a common procedure among those with severe coronary artery disease, and is performed in efforts to improve blood flow to the heart in the case that multiple coronary arteries are narrowed or blocked with plaque buildup.
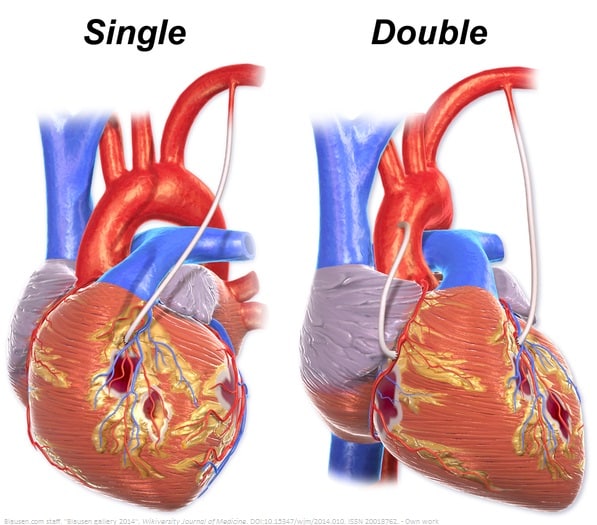
Patients who undergo the standard incumbent procedure have an artery harvested from their chest or leg. Immediately after, it is surgically mended from the aorta to the coronary artery, acting as the bypass around narrowing or blocked arteries of the heart (see image). This mode of procedure is very effective as it has been perfected over four decades and the grafts typically last 10 to 15 years.
Despite the effectiveness and consistent success of the standard procedure, a few innovative companies have tested a synthetic conduit to act as the bypass around narrowing or blocked arteries of the heart.* Clinical trials for this type of innovation have been performed for the purposes of CABG, but that is as close to market this technology has made it, to date. If adopted, the synthetic conduit will simplify the CABG process and make it less invasive by eliminating the need to perform a separate surgery to harvest a blood vessel. However, despite its simplicity, if innovators are successful in bringing this synthetic graft to market, it will begin as an inferior option and pose a greater risk of complications relative to harvesting an artery. It would then take years of sustaining innovation, incrementally improving product performance over time to better meet patient demands, for its outcomes to outperform that of an actual artery. So, why would a physician or patient choose the synthetic disruptor option in the first place if the incumbent process is associated with a lower risk of serious heart complications?
Well, those who have the option of choosing the incumbent procedure won’t choose the synthetic graft. But, there are patients with severe coronary artery disease whose lives could be bettered with CABG, but do not have viable arteries or veins for harvest (and are not eligible for angioplasty). This is a common circumstance among patients who need reoperation or multiple bypass surgeries, but viable arteries for grafting have already been used. This circumstance is also apparent when the patient’s candidate arteries for grafting have been damaged or determined inaccessible. Patients in these categories are unlikely candidates for the incumbent CABG procedure, and thus are the nonconsumers that the new market is expected to contain.
These nonconsumers still have the same job of improving blood flow to their cardiac tissues as those eligible for the incumbent CABG procedure, and now they have a potential solution in the disruptive synthetic conduit. In their circumstance, the synthetic conduit is competing against the risk of not intervening at all, because the incumbent method of harvesting an artery for bypass is out of the question for them.
If successful, this hypothetical synthetic conduit will then have found a foothold market upon which innovators could, over time, perfect and improve upon its performance and integration into the process of CABG. With sustaining innovations to the synthetic conduit and other enabling innovations in biomaterials —like improvements in 3D printing technology—the disruptor could eventually rival the incumbent CABG procedure in valued performance metrics. The need to perform a separate surgical procedure to harvest an artery may be eliminated, potentially improving costs, time, and patient experience.
Potential impact
By focusing product development efforts on the patients whose circumstances prevent incumbent technologies from meeting their health needs, disruptive entrepreneurs can establish a foothold market in which to sustain and improve their technologies over time. Within this relatively visible area of nonconsumption, potential disruptors can avoid direct competition with well-established incumbents until their performance begins to rival that of the incumbent’s. This increases their likelihood of competing effectively in the long-term. By establishing a foothold market of patients in exceptional circumstances relative to mainstream patients, new-market disruptive innovations empower our healthcare providers to provide viable treatment options, and along with them, hope and promise, to a greater number of patients who otherwise have nowhere to turn.
—
* The astute may notice that the synthetic conduit is a sustaining innovation relative to coronary artery bypass grafting (CABG). This is a correct assessment. Disruption should always be thought in relative terms. The synthetic conduit is disruptive technology relative to the artery harvesting technology within the CABG process.



