Spiraling healthcare costs have been of grave concern to the healthcare industry, government, and public for at least 50 years. And while the debate remains heated over the appropriate strategy for addressing them, there is one fact upon which many analysts agree: There can be no solution to the healthcare crisis that does not address America’s unchecked epidemic of chronic disease. Chronic conditions afflict more than half our citizens and consume 86% of the exorbitant $3.2 trillion spent each year on care.
To prevent and reduce the cost of managing chronic disease, providers must learn to facilitate change in individual behavior, which has the greatest impact on health of any contributing factor, including healthcare. How can they do that? By tapping into consumers’ Jobs to Be Done.
Jobs Theory explains that people don’t actually want what marketers are selling, per se. They want to make progress in their lives—however they define it—and they do so by “hiring” solutions in various forms, from products and services to life and work experiences. The key for healthcare providers, then, is to discover the progress patients are already trying to achieve—their Jobs to Be Done—and craft health treatments and regimes that helps them achieve it . Unlike many traditional healthcare solutions, jobs-based solutions are also built to align with patients’ unique circumstances and goals. Thus they’re easier for patients to embrace, and can help them become more effective collaborators in their own care process.
Take for example, “Sabeena.” She’s 34 years old, has two children, and works as an IT service team leader. She used to play basketball in high school, but she gained the “freshman 15” at college, and another 30 pounds during each of her pregnancies. As a result, Sabeena has high blood pressure, difficulty breathing, poor mobility, and frequent pain in her knees. She remembers how good it felt to be fit, and worries she is now a bad example to her children.
Prevailing chronic care practices would lead physicians to classify Sabeena according to her clinical diagnoses—obese, hypertensive, pre-diabetic—and prescribe solutions proven effective for the “average” person with similar diagnoses. These might include medication to lower blood pressure and mitigate knee pain, coupled with exercise and healthy eating to promote weight loss. Then Sabeena would be expected to incorporate the new drug regimen into her life, and find and follow a weight-loss program on her own.
Hence the problem. These prescriptions require a high level of self-management that Sabeena might find difficult to attain, given the unique barriers to healthy behavior she grapples with every day. These include her parenting duties and varying shift schedule, which make promptly picking up medication renewals difficult, and routine exercise all but impossible. Then there are the free, cheesy hot lunch buffets wheeled into the staff lounge most weeks to reward team performance, which save her time and money. She lacks health-savvy friends and colleagues to mentor her in adopting healthy habits, and she’s afraid to try and fail again. And, at the end of the day, she lacks the emotional bandwidth to invest in anything beyond her highest priorities: her children and her work.
Sabeena needs more than just clinical solutions. She needs holistic health solutions that help her make progress in context of this broader web of circumstances.
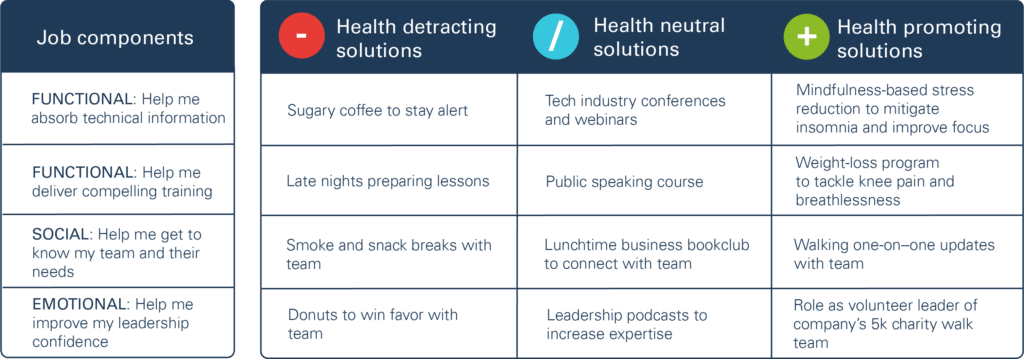
How would healthcare professionals take a jobs-based approach to helping improving Sabeena’s long-term health? They’d uncover the jobs arising in Sabeena’s day-to-day life that cause her to hire unhealthy or health-neutral alternatives. They’d then work with Sabeena to create healthy solutions that address the functional, social, and emotional components of those jobs and fit her unique circumstances.
For example, one important job Sabeena is hiring for is “help me excel at training my team.” To make this progress, Sabeena must be able to absorb a constant stream of emerging technical knowledge. This requires a high level of mental alertness, which she currently attains by drinking six cups of sugary coffee a day. So from a functional perspective, a jobs-based solution would offer Sabeena a healthier means of staying alert, like mindfulness techniques to mitigate her insomnia. Importantly, that solution would result from a robust dialogue between her and her provider about the reasons behind her behaviors, which she must understand in order to consistently identify and embrace healthier alternatives.
Training also requires a compelling communication style that Sabeena has struggled to develop. A health solution for Sabeena’s Job to Be Done, then, might reduce her knee pain so she could comfortably walk around the training room to engage more directly with trainees, rather than teaching from a seat at the front. It might also seek to improve Sabeena’s breathing, which is labored due to her excess weight, so she could speak in a more audible and assured manner. A well-supported weight-loss program designed to fit with Sabeena’s circumstances might be such a solution.
From a social standpoint, a jobs-based health solution would connect her with peers also trying to improve their health, so they could share encouragement and ideas for overcoming day-to-day obstacles. Emotionally, a health solution would need to feel achievable, and progress would lead not only to health improvements, but to a sense of accomplishment that could improve her confidence and performance on the job, too. Leading the company’s 5k charity walk team would fit those criteria, so long as the time-commitment was feasible for Sabeena.
Solutions for Sabeena’s job: “Help me excel at work”
People lead complex lives, grappling with myriad responsibilities and circumstances that sometimes keep them from acting in the best interests of their health, particularly where chronic disease is concerned. Providers can unleash patients’ potential to manage it more effectively and independently by working with their existing Jobs to Be Done, rather than trying to work against or change them.
See our research on applying Jobs Theory to healthcare:
Health for hire: Unleashing patient potential to reduce chronic disease costs


