April 24th-30th was National Infertility Awareness Week in the United States. But for an issue affecting 12% to 20% of couples, it should get more than one week of attention. In light of its impact, I’m highlighting three women’s health issues around infertility and why so many still do not receive treatment.
The first issue is the cost and inaccessibility of infertility treatments. In the US today, there is an immense amount of nonconsumption of fertility services due to lack of insurance coverage, the cost of medications, and limited access to providers. As of April 2021, only 19 states had laws requiring infertility insurance coverage, with only 13 including in vitro fertilization (IVF) coverage. Additionally, a 2017 Mercer study found that only 56% of large employers – those with 500 or more employees – cover any type of fertility service. However, most do not cover IVF, intrauterine insemination (IUI), or egg freezing. More employers cover evaluations for infertility diagnosis and medications.
While it’s nice to get a diagnosis, that only gets one so far. A diagnosis may lead to the need to invest thousands of dollars to address an identified issue, which creates a barrier many cannot overcome. Below is a chart highlighting the out-of-pocket costs of infertility treatments and successful outcomes, which you will see range from $1,200 to $73,000. This data is from a 2019 report, so costs have likely increased.
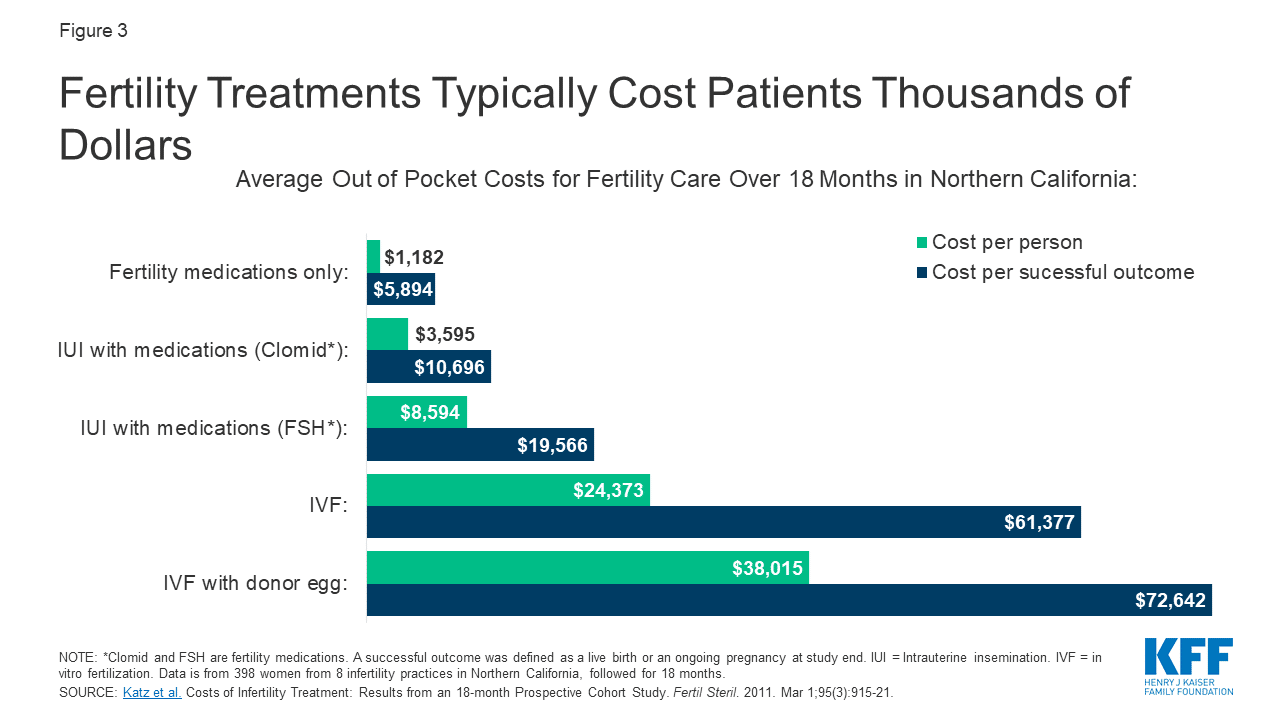
With price points this high, many individuals have no alternative but to be nonconsumers of care. Given the complexity of fertility struggles, and the technology and expertise required to address it, the industry is still highly centralized. This requires women and couples to seek out the required expertise, usually in the form of reproductive endocrinologists. Their services are not only expensive, but their numbers are limited. Innovators are starting to break into the market, but there is a long way to go before access and affordability are achieved at scale.
A second issue that calls for more attention is female physician infertility. It plagues around 25% of female providers. A woman’s most fertile years and medical careers do not align well for pregnancy and new motherhood. Many women have children during critical phases of a physician’s career: training or early career practice. And for women seeking to undergo fertility treatment, there is a big conflict with work schedules. To ensure there is a doctor present to see patients, most practices require advanced notice for physician time off. But this isn’t how fertility treatment works. Treatment schedules are unpredictable, as they depend on individual responses to medication and hormone levels, which change daily. As a result, many providers are forced to choose between their practice or pursuing treatment. Many female physicians are starting to speak out about infertility struggles in the physician population. You can read more on the scale of the problem here, here, and here.
Third, in addition to the financial and physical toll infertility takes on individuals, the mental health burden is significant. Searching #infertilityawarenessweek on Twitter reveals stories that range from sad, to horrific, to hopeful as women share their infertility journeys. While around 30% of issues are of male origin, very few men seem to speak out about it. It’s a shameful topic. Over a decade ago, Harvard Medical School identified similar levels of depression and anxiety in patients experiencing infertility as those diagnosed with cancer. Shame, anxiety, depression, loneliness, and exhaustion plague many individuals going through treatments, as well as those who cannot access them. Due to the cost of mental health services, there is additional nonconsumption of care for secondary health issues like the mental burden of infertility.
While the current reality of infertility’s population impact, cost, access struggles, and secondary health concerns may paint a grim picture, the story isn’t finished. As theory would predict, many innovators are already seeking to serve the nonconsumption in the market. Recently, Alife Health, an AI-enabled clinical decision support tool to improve the IVF success rate, received $22M to launch its product. They aren’t alone. Overture Life IVF is an innovator seeking to simplify the entire IVF process through automation, making it more affordable, accessible, and successful.
Time will tell if these innovators will succeed. In the interim, their launch and growth highlight the market demand for more affordable and more accessible solutions for some of women’s health’s most pressing issues.



