A mere two years after COVID-19 shut down the country, we were slammed with another public health concern: monkeypox. As of mid-August, there were 14,115 confirmed cases of monkeypox in the US. While the disease burden is not nearly to the same scale as that of COVID-19, the global spread of monkeypox is enough for the WHO to have it declared a global health emergency—the second in two years.
In fact, we’re seeing a lot of the same issues with monkeypox that made COVID-19 so difficult to contain. Cases are rising, despite limited access to tests and data on its spread. And even though vaccines rolled out far quicker than the COVID-19 vaccine, current supply is not meeting demand. In early August, the FDA approved a plan to split a single monkeypox vaccine dose into five doses, which expands how many people can be treated; however, this will not fully solve the dose shortage, and the manufacturer is worried about the plan’s safety.
COVID-19 rocked our health care system, highlighting all of its flaws in vivid detail. Now, we’re seeing the fatal flaw of the US health system yet again: we are so focused on treating illnesses as they arise, rather than preventing and containing illnesses, that we are not equipped to tackle a public health crisis of any scale.
There are many who say that the answer to this problem is investing in public health infrastructure and funneling resources into an already stretched thin public health system. As a public health professional, I agree that it’s important to fund public health efforts far beyond the current level. But to say increasing public health investment will put us in a better position to tackle the next public health crisis is a misdiagnosis of the problem. It’s not just a lack of funding that is the issue—the entire health care business model needs an overhaul.
Business models and the health care system
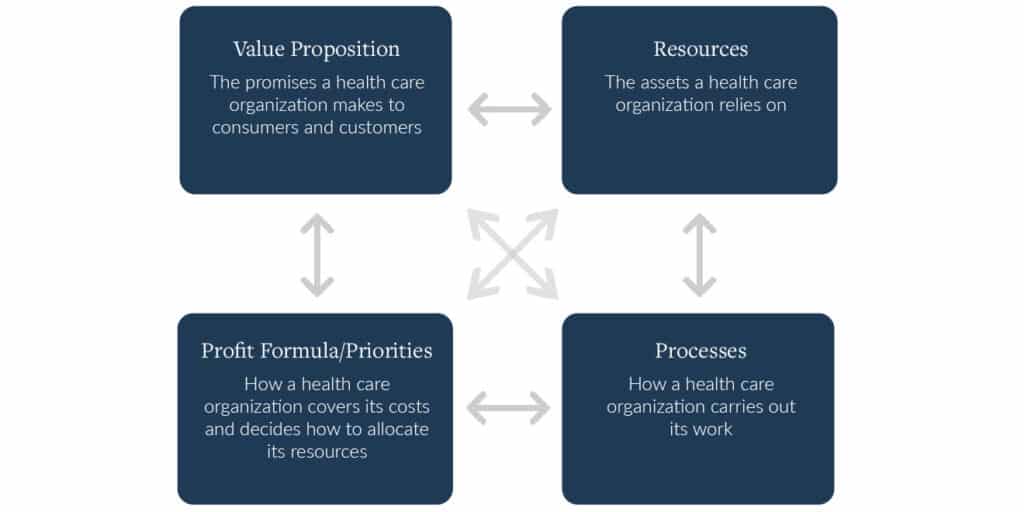
Business models are comprised of four interdependent elements that, taken together, create and deliver value. Each element of a business model is important in its own right, but the business model is how those four elements interact with each other.
Figure 1. The four components of a health care business model
The business model of health care in the US is heavily focused on treating illnesses. Many hospitals, often seen as the beacon of the health care system, proclaim they have the medically advanced ways to treat illnesses, with set processes to fulfill that promise. Most health care resources, including money and equipment, go to the goal of revolutionizing medical treatment. This is all wrapped up in a fee-for-service reimbursement model, which incentivizes volume of services provided over the value services create. I previously wrote, during the height of COVID-19, that the health care system’s specific focus on treatment and volume, rather than prevention and value, was a main factor in the country’s struggle in controlling the pandemic.
Because the health care system focuses so much on treatment, prevention is often ignored and undervalued. Less than 3% of health care spending in the US goes to public health efforts. The business model of health care is so tightly woven around treatment, that a change in only one of the four components (value proposition, resources, processes, and profit formula) is ineffective, because it goes against the core goal of the business itself. Even now, the CDC is changing COVID guidelines to focus less on preventing disease spread and more on treating the illness, showing where the focus of US health care is directed, even in regards to a pandemic.
What all of the analyses criticizing our public health response seem to be missing is that we need to change the business model of health care. It must be characterized by a model that has the resources, processes, and priorities to tackle emergent public health emergencies before they start or as they start, rather than scrambling to contain them once they get too big.
Investments in prevention and public health efforts will be a valuable part of a business model overhaul, but it is not enough to simply funnel money into providing prevention-oriented resources. For US health care to be better positioned to address the next pandemic, all four business model elements need to shift to focus on prevention; otherwise these additional resource investments will be fruitless. Without all components of the business model working in lockstep towards the same goal, there will be no return on prevention investments.
As it stands, the health care system is doomed to repeat its mistakes the next time there is an infectious disease outbreak. Unless there is a transformation in health care’s business model, to prioritize prevention of outbreaks over treatment, this pattern will not be broken. The result, unfortunately, is that we will be living out the definition of insanity – doing the same thing over and over again and expecting a different result.