Depression is a devastating illness that troubles up to 7% of the U.S. population in any given year. Drug treatments such as Zoloft and Prozac have become household names – yet good evidence suggests that these SSRIs are only barely better than a placebo, and that’s when they work at all. Coupled with a second treatment, prospects are slightly better. But only slightly, and side effects are worse.
At the same time, potentially revolutionary treatments are struggling to gain traction:
- Exercise appears to be an effective therapy for treatment-resistant depression, encouraging remission when drugs just don’t do it. But, unlike the doctor in the article, most doctors don’t prescribe exercise to depressed patients.
- Ketamine, a relatively low-cost sedative with a long safety record, effectively lifts severe depression in hours for many patients. Yet every article on ketamine treatment quotes doctors cautioning against administering this potentially life-saving therapy, suggesting that it will be years before an FDA-approved on-label medication hits the market.
- Transcranial direct-current stimulation (tDCS), or using an extremely small current from a 9-volt battery to noninvasively stimulate the brain, actually makes Zoloft more effective than a placebo. It also appears to increase creativity and focus. But despite its low risk and low cost, experts are doubtful that this treatment will quickly hit the market – if it ever does.
Why do some inexpensive yet effective treatments struggle to come to market while other ineffective but expensive treatments thrive? The answer, along with potential solutions, lie in understanding the health care value network.
What is a value network?
A value network is “the context within which a firm establishes a cost structure and operating processes and works with suppliers and channel partners in order to respond profitably to the common needs of a class of customers.”
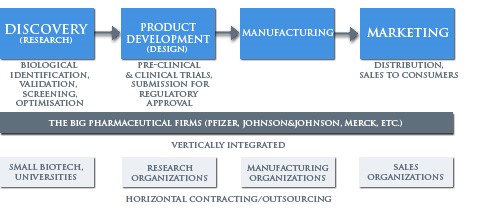
Unlike a value chain composed of win-lose upstream and downstream relationships, value network implies economic incentives and business models that are mutually reinforcing. In the pharmaceutical industry, for instance, the value network often looks something like the (simplified) diagram below.
Source: https://web.duke.edu/soc142/team2/shifts.html
The value network allows each of these groups to make money in distinct ways. Small biotech firms sell their discoveries (and themselves) to larger integrated firms that can afford the clinical trials and marketing necessary to bring a drug to market. Integrated firms contract out to other groups for some of the development and marketing work. In the US, the FDA establishes processes for regulation and approval. Each of these pieces reinforces the others.
The value network simultaneously welcomes technologies and business models that enable it to make money and excludes technologies and models that undermine the network. Take ketamine depression treatment, for example. Because the drug is no longer patented and is easily manufactured, no group in the value network can make money off of its development, and thus no group is sponsoring FDA-required trials for ketamine treatment of depression. AstraZeneca, however, is running trials of a ketamine-like drug that could be patented and sold at higher rates. Of course, the drug is not as effective as ketamine itself. But it supports the value network.
Encouraging new value networks in health care
Fortunately, there are ways to reshape old value networks and to create new ones. Reshaping old value networks often takes a tremendous degree of discipline and incurs large costs, but creating new value networks through disruptive innovation has a long track record of lowering costs and increasing accessibility to innovation. Here are two ways that disruptive therapy-enabling value networks could emerge:
1. Deploy disruptive therapies by targeting nonconsumption
CPR was first deployed only in hospitals, but spread rapidly to mobile clinics, then to first responders, and finally to people with no formal medical training. While its effectiveness is questionable in some populations, the spread of CPR shows that low- or no-cost therapies can be widely adopted. CPR could spread for two reasons.
- It did not compete against incumbent health care providers. In fact, it increased patients seen by established professionals.
- CPR use targeted nonconsumers, or those who were neither providing nor receiving health care – individuals without medical training, and people in cardiac arrest that the health care system could not help.
Deploying effective low-cost therapies by targeting current nonconsumers is one of the only ways that value networks can evolve. Low-cost treatments are unlikely to make inroads with incumbent businesses and care providers, but they can explode when first targeted to nonconsumers or the low-end of the market (the most troublesome and expensive individuals).
2. Enable unique regulatory pathways that lower barriers to potentially disruptive therapies
Polycystic kidney disease patients were recently deprived of an effective life-preserving medication because of potential side effects in a limited number of trial subjects. All-or-nothing drug approval supports the current drug therapies value network: had the kidney disease drug been approved, the FDA and pharmaceutical companies may have been liable for the very small number of adverse cases that occurred. Alternate regulatory paths, perhaps ones that place more emphasis on risk mitigation strategies while easing approval requirements, could encourage value network shifts that would make effective treatments more accessible.
3. Create businesses that integrate around diseases rather than industry stage
The industry-segmented value network (discovery->development->manufacturing->marketing) is quickly becoming commoditized. This value network relies on treatment-specific reimbursement from payors under a fee-for-service model. Business that integrate around treating a disease end-to-end, on the other hand, have a unique opportunity to utilize effective, low-cost therapies. A depression-targeted company, for instance, could say, “Pay us $X and we will provide all of the necessary equipment, medication, training, etc needed to treat this disease.” This company would be incentivized to provide effective care at the lowest cost, and brings demonstrable value to providers already squeezed by shifting reimbursement frameworks.
As innovators follow these principles, we are confident that low-cost effective therapies can make healthcare more affordable and accessible by revolutionizing disease treatment.