When following the news, we sporadically hear about new medical breakthroughs that leverage advanced technology, like gene therapy, to give new options to patients suffering from diseases that we have yet to develop an adequate treatment for, such as multi-gene disorders. But, when we hear about these breakthroughs, how long does it take before they are truly within reach for the public?
The most perplexing and complex medical problems of our time are combated with advanced technology and expertise, typically so complex and expensive, only people with the highest degrees of skill and institutions with a lot of money can own and use the equipment. To economize on the scarcity of money and skills, activity in these industries become centralized—meaning we must take the problems we’re trying to resolve to a central location, where people with the requisite expertise and equipment can solve them.
Being centralized is not the ideal nature of a capability. Inconvenience and high price commonly end up being formidable barriers to use for a public itching to take advantage of the new technology to make their lives better. In healthcare, we attempt to overcome the price barrier with insurance, which in some cases covers a significant portion of the price. But, this results in greater spending than would otherwise be the case, and does not address the barrier of inconvenience.
Luckily, things don’t need to remain this way. The high cost and inconvenience of immature and centralized technologies are typically quick to be identified by innovators, who begin to build new ways to decentralize the technology and its capabilities. When this is accomplished, technologically advanced solutions are no longer confined to hospital walls. Instead, they reach closer and closer to the day-to-day circumstances of individuals. Technologies and new capabilities mature from cumbersome to practical in this manner.
For example, the first technologies developed for testing a patient’s blood glucose levels were located only in hospital labs. Patients had to travel to the hospital, where trained technicians operated machinery that analyzed blood samples for blood glucose levels. Over time, the capability to measure blood glucose was decentralized to doctor’s offices, and now patients have portable meters in which they can measure their levels on-the-go.
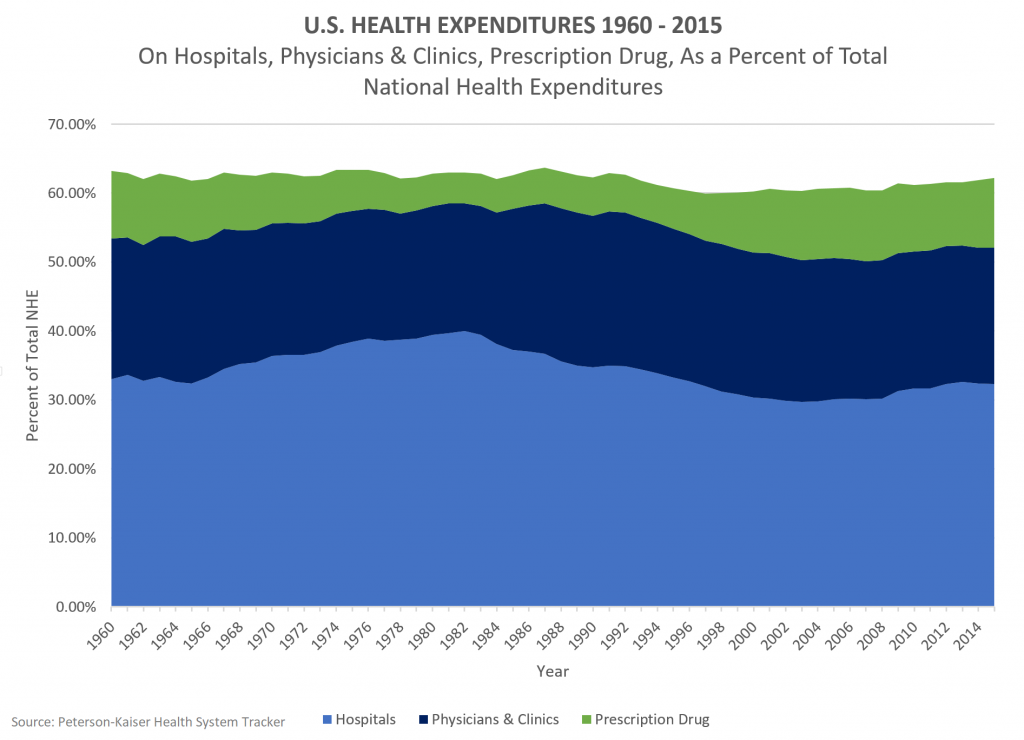
Despite the many examples of formerly advanced medical technologies being decentralized, our healthcare expenditures at the hospital have remained relatively consistent over the last 50 years as a proportion of total national health expenditures (see below). If medical technologies are truly diffusing away from the hospital to lower costs and more convenient sites of care, something else must be going on to prevent overall hospital expenditures from decreasing.
1) Are hospitals continuing to adopt cutting edge technologies that expand their capabilities?
This is the best case scenario for explaining our hospital spending. If novel, advanced technologies are continually being adopted by general hospitals at the same rate in which other capabilities are diffusing away from hospitals to other sites of care, then we won’t be reducing hospital expenditures (but at least we’re building the capabilities to meet the needs of more people).
2) Are procedures that could be done at a lower cost elsewhere getting hung up, and not diffusing away from the hospital?
The number of hospital outpatient department visits per capita have increased over the last two decades, while the number of hospital inpatient days per capita have decreased over the same period. This uptick in hospital outpatient visits is significant, because hospitals are paid, on average, 85% more for a given outpatient procedure than an ambulatory surgery center. May this price discrimination be pushing hospitals to cling to medical procedures that could potentially be performed at lower priced facilities?
These are important questions to consider as innovators continue to work to make medical technologies less complex and accessible. Healthcare leaders must in turn address whether these medical innovations are making their way to more affordable and convenient to access sites of care.
What else could account for the disproportionate amount of hospital spending in the U.S.? Comment below.
For more, see:
How Disruption Can Finally Revolutionize Healthcare