The pandemic highlights a point Clayton Christensen made over ten years ago: the predominant business model of general hospitals is not sustainable.
Throughout the COVID-19 crisis, many hospitals have been losing money. The American Hospital Association estimated in May that hospitals in the aggregate are losing up to $50 billion per month. Healthcare workers are facing furloughs and are being laid off, and rural hospitals, already in a precarious position, are being forced to close.
While the virus forced many types of businesses into distress, its impact on hospitals reveals pre-existing problems with the general hospital and its role in the broader US healthcare system.
In The Innovator’s Prescription, Clayton Christensen and his co-authors explained that the hallmark of the general hospital business model is its aim to serve all health needs under one roof. In order to do this, hospitals manage two different business models in the guise of one, a feat that ultimately adds complexity and cost to the healthcare system and patient experience.
General hospitals’ broken business model
General hospitals provide value for patients in two ways. One is diagnosing diseases and medical conditions when presented with a set of symptoms. Diagnosis relies heavily on resources and expertise, and works well under a fee-for-service payment model because there is no definite, cut-and-dry procedure 100% of the time. Some medical conditions may be picked up by a simple MRI, but others may take weeks or even months of testing to figure out. Doctors are therefore compensated for the work that goes into a still intuitive practice.
The other way hospitals provide value is by treating health issues as quickly and effectively as possible, which functions best with a fee-for-outcome payment model since results are more process-based and easily guaranteed. For instance, a joint replacement can follow reasonably predictable steps from beginning to end. The amount of work that goes into the procedure, as well as the outcome of that procedure, can be quantified into a set price.
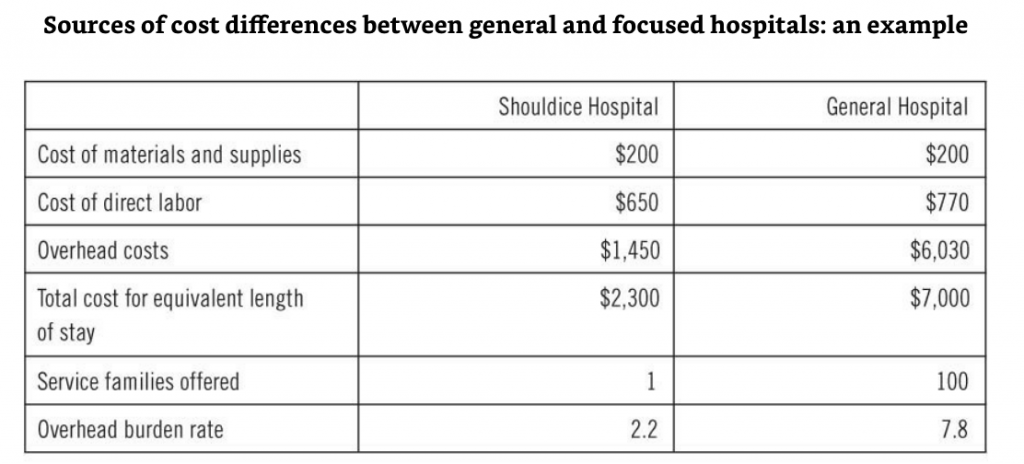
Ideally, each of these critical services would operate independently from the other since they are most efficiently covered by distinct business and payment models. Unfortunately, combining the two under one roof forces both to operate under a fee-for-service payment model (in most cases). Significantly, it also results in a duplication of resources and processes as they work to accomplish different goals. The end result is a dramatic increase in overhead costs (like billing and administrative costs) that aren’t directly attributable to patient care. These are spread across departments, make up a massive amount of healthcare costs, and are ultimately passed on to the patient.
The table below highlights the difference in overhead generated by a general hospital in comparison with a focused, single-procedure hospital that doesn’t conflate multiple business models.
Hospitals’ achilles heel: Over-reliance on treatment
Whereas diagnostic work generates a lot of overhead costs due to the trial and error aspect of the work, treatment is far less costly for hospitals since procedures are predictable and use only what’s absolutely necessary to deliver results. This dynamic has led to hospitals’ achilles heel: an over-reliance on high-volume treatment procedures that offset the burden of costlier diagnostic departments.
In the context of the current pandemic, this has spelled disaster for the general hospital. In order to protect patient safety, most hospitals cancelled or postponed all elective procedures—surgeries that, while in many cases necessary, did not need to happen immediately. Losing out on the income from profitable procedures that hospitals depend upon, like hip and knee replacements, has left them vulnerable. Without a mechanism for offsetting the high overhead costs that diagnostics generates, even the busiest hospitals have struggled to remain operational.
The fatal flaw of the general hospital is its attempt to provide everything to everyone. During a pandemic, this means most hospitals have trouble keeping the lights on. Outside of a pandemic, it means that patients are likely paying far more than the true value of their healthcare.
What COVID-19 shows is that hospitals are just one healthcare catastrophe from shutting down—which would be a disaster for patients everywhere. What’s needed is a fundamental rethinking of the role of general hospitals in our healthcare system, and how the services they provide can be more efficiently carried out in order to reduce the cost of care for all parties.